Posts tagged ‘trigger point’
Important muscles involved in hand, wrist & arm pain – Part 1
There are many intricate muscles and soft tissue structures in the hand, wrist and arm which can cause various types of pain, numbness sensations, weakness, pins and needles or electric shock type of sensations when they become constricted, tight or dehydrated through physical over use or misuse, bad posture, accidents, old injuries (such as high velocity neck impact or whiplash) and deep scar tissue, and/or combined with unremitting emotional stress.
2 muscles which I’d like to draw the reader’s particular special attention to in this article are the scalenes and pectroalis minor muscles. These are 2 very important and relevant muscles which massage therapists who have been through advanced trainings in say for example clinical massage techniques will know how to treat efficiently and very specifically. Both of these muscles are very much neglected in most general relaxation massage work. The scalenes muscles are located in the base of the lower neck and attach to the first and second ribs, whilst the pectoralis minor muscles covers the 2nd, 3rd and 4th rib in the region of the front upper chest. Both muscles although located respectively in the neck and upper shoulder region are often highly relevant in hand, wrist and arm pain pathologies, one of the main reasons behind this is that the brachial nerve plexus and its subsequent other sub branching nerves serving the arm passes directly underneath both of these muscles so any tightness in either of these muscles is going to have a direct physical effect on creating nerve related aggravation in these regions.

[Trigger Point Pain Referral Pattern for Scalenes Muscle Group]

[Trigger Point Pain Referral Pattern for Pectoralis Minor Muscle]
Signs of nerve related impingement or over simulation can include pins and needles, intermittent shooting pains over a certain region (such as down the arm), electric shock type sensations, or areas of numbness. Nerve impingement caused by the scalenes or pectoralis minor muscles can also cause the muscles and proprioception to misfire so causing symptoms of weakness or spasm in the arm, hand or wrist. Symptoms of carpel tunnel or other repetitive strain injury type side effects can also be triggered or caused by soft tissue tension in these apparently unrelated areas further up and away from the hand, wrist and lower arm (but which you now know after having read this article and viewing the related videos are very much related).
Tightness in the scalenes muscles can cause tingling all the way down to the thumb and first fingers of the hand, whilst pectoralis minor tension cause refer tingling all the way down to the ring finger and little finger. Constriction of the blood supply serving the arm from a tight pectoralis minor muscle can also cause feelings of coldness or lack of circulation to the fingers.
Habitual shallow breathing, particularly whereby the type of breathing only involves the use of the upper chest (rather than full deep belly breaths) is another potential cause of chronic tightness in the scalenes muscles. Stress management through gradual build up practice of proper relaxing deep breathing is the perfect antidote. Notice when you’re stressed or shallow breathing, be gentle and kind to yourself, congratulate yourself for noticing and just start by receiving 3 deep breaths in and out and build up that number over time, the idea is that over time it builds up to more of an unconscious habit rather than a conscious effort.
As with all these topic, there’s always so much that could be written or linked to, this is just what I could cobble together off the top of my head and without turning this into a fully blown dissertation as well as given the fact that I would like to go to bed in a moment (!!), but if you want to know more or have any suggestions I would be glad to receive your feedback as always and compile a part 2 or further subsequent parts as a follow on to this particular article as the demand unfolds.
Be well! 🙂
Email: info@isca-therapies.co.uk
Visit the ISCA Therapies website: www.isca-therapies.co.uk
Resolving back pain through spinal manipulation
(1).jpg)


Important Muscles Involved in Lower Back Pain – Part 2 : Psoas

The Psoas muscle is one of the most commonly involved yet under treated muscle in lower back pain conditions, save to say it is probably the number 1 missing link in a lot of cases where the muscle has never been directly addressed and appropriately rehabilitated in many cases of unresolved lower back pain. Due to the relatively deep location of the main fibres of the psoas muscle, it is seldom treated directly unless the practitioner concerned has had training in the appropriate techniques. The muscle itself covers a very large area of the lower back and pelvic areas, significantly it attaches to the front facing side of each of the lowest set of 5 vertebrae bones of the spine, continues on to lines in the inside of the pelvis (where it is sometimes becomes known as the “iliacus” muscle) and finally attaches to the top inner part of the femur (aka tigh bone). Due to its attachment to the front of the lower spine, tension in the psoas muscle can pull the spine forward causing an excessive forward curvature in this region (known as an excessive “lordosis”) which in turn causes the opposing muscles attached to the back facing side of the spine to become over stretched and over tensioned (muscles including the quadratus lumborum and other spinal muscles which we discussed in part 1 of this article series).
As can be seen from the above diagram set depicting the trigger point pain referral patterns for the psoas, the first illustration shows the pain pattern for the back of the body which is essentially quite straightforward as it is just a localised pattern (relative to the absolutely position of the psoas muscle itself) running parallel along either side of the lower part of the spine. The second illustration however might be a surprise as it shows pain referral which can get set-up and experienced on the front of side of the body which in this case is a region around the inner groin and inner thigh area, so anyone experiencing pain in these areas it’s possible to attribute this to trigger points in your psoas muscle. Proper and thorough treatment of the trigger points in the psoas muscle requires that the practitioner goes in gradually and eases in deeply moving the intestines aside in order to make contact with the psoas (and iliacus), the direction of aim is toward the spine in order to work directly on the psoas (but not ultimately to make contact with the spine). This procedure need not be excruciatingly painful for you the client so long as your practitioner maintains a “listening sense of touch” at all times, as well as working slowly and gradually in rather than forcing their way in with battling haste and impatience.
The following video gives a nice interactive over view of the anatomy for the psoas muscle and gives a few pointers on what issues may arise as a result of the psoas muscle being overly locked in tension or on the flip side in weakness (which is generally rare):
So, here is our first video showing you a classic de facto standard stretch for the psoas muscle, note that a varation of this stretch can also be done whilst lying totally flat on the floor i.e. the leg that would have been hanging off the edge of the bench in the video example would instead be stretched out straight flat against the floor instead:
Now, here are 2 alternatives… The first variation is a stretch that can be performed standing (instead of lying down):
The second variation is a bit more complicated to grasp, but fine once you’ve understood what you’ve got to do! This video was for me personally a very interesting stumble upon as it’s is based upon the paradigm of myofascial stretching. I myself perform myofoscial release work for releasing individual muscles, but have never really looked into studying myofascial stretching before and has thus whetted my appetite, so any comments welcome about this from either total new comers or those experienced in myofascial stretching already. I tried the exercise in the video below for the first time earlier on just before writing this article and it is certainly effective yet gentle and holistic (i.e. you can feel other parts of your body gradually and subtly freeing up as well during the stretch process) all at the same time:
Remember, if you have on-going lower back pain and have never had your psoas muscle properly treated for trigger points and properly (myofascially) released by a suitably qualified massage or physical therapist, chances are that this is exactly what the missing link is.
Take care for now and see you for the part 3!
Important Muscles Involved in Lower Back Pain – Part 1 : Quadratus Lumborum

This Quadratus Lumborum muscle is perhaps one of the most relevant yet not always adequately treated muscle by healthcare practitioners who work directly hands-on with the body’s physical structures in relation to attempting to resolve lower back pain conditions. I will bring to your attention other relevant and important muscles involved in lower back pain and movement restriction issues in this series of forthcoming blog articles. These articles will feature informative videos that I have come across on YouTube giving an introductory overview of the relevant anatomy background followed by useful self help stretching exercises to facilitate release of tension in the muscle being reviewed.
In the above image, drawing C illustrates the anatomical positioning of the Quadratus Lumborum muscle, note that this muscle is actually semi deep and beneath another group of muscles called the Erector Spinae group which sit directly on top. Drawings A and B illustrate the pain referral pattern that can get set-up when there are trigger points in this muscle, as is usual with the phenomenon of trigger points the actual apparent location of the pain or soreness experienced as defined by the shaded areas in the above diagram is referred i.e. it’s possible that no pain maybe directly felt in the muscle itself even though micro tension knots in the muscles itself are causing pain to be referred and felt in the buttocks.
Here’s an interactive anatomy lesson and an example of some exercises you can do to help stretch and free up this muscle, although to do them requires additional equipment (a swiss ball) and would not be recommended to an absolute beginner:
The self help exercises which follow in each article must feel comfortable to do at all times, there is no useful benefit to be gained and the chance of injury to occur by pushing yourself into any discomfort or further pain. Also, remember to breath in deeply and breath out just as you’re about to go into the stretch, many people commonly (and unconsciously) hold their breath as they are about to perform stretches find that they can go a lot further as well as with less resulting pain after changing over to breathing properly as suggested.
So to finish off with, here are some simple exercises which do not require additional equipment and can be done by most, if not all when adapted to within your tolerance level.
The exercises should ideally be performed daily as part of a rehabilitation program and in conjunction with regular visits to a suitably qualified massage or physical therapist who can perform the supporting release or soft tissue manipulation work on the muscles involved.
See you in part 2! Take care now.
Freeing up the shoulder and opening up the rib cage!

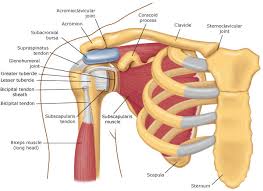
Treated a client today who came in barely able to internally rotate her right shoulder girdle and had given up doing even light exercise due to stiffness all the way down the back as well pain next to the shoulder blade which onsets when reaching her arm up.
We worked on the major shoulder girdle muscles, in particular worked on Teres Minor which was very tense and tender at both attachment points (i.e. outside edge of shoulder blade half way down and top of the arm – to use non technical anatomical descriptions) . Also did fascial release work on serratus anterior muscle on the side of the rib cage. Client was feeling slight burning or crackling sensations as the taught and dehydrated connective tissue (fascia) began to yield and begin to give us back some flexibility to allow movement to happen more freely. We ended up with greatly improved range of movement afterwards.
Wondered and asked client if she suffered with asthma as the intercostal muscles in-between the outside surface of the ribs seemed very restricted from what I was able to palpate (feel) during the time that we were working on serratus anterior, she confirmed that she did have asthma. I explained that there is a set of techniques I can perform on her during a series of future sessions in order to free up the currently restricted muscles and soft tissues of the rib cage which will help ease the asthma and help free up the breathing making it become less shallow.

Are trigger points the answer to your unresolved soft tissue pain?
Almost immediately after I had completed my initial basic training in massage, I happened to come across across a series courses for already qualified therapists such as myself, the courses were modular and taught remedial soft tissue techniques and skills to profoundly affect soft tissue pain conditions for the better in clients. This new information opened up a whole new range of clients for me whom I’d never have thought of working with before and changed the course of my practice. Trigger point therapy along with myofascial release are the joint top 2 remedial techniques that appear to have the most profound affect on clients I have worked with, especially ones who have been around the houses already to see conventional health professionals and other alternative therapists without much of a result.
Trigger points are basically a single point of very tight knots in the fibres and fascia (connective tissue) of a muscle which causes pain to be felt as result, these knots can vary in size from a pea to a grain of sand. An appropriately experienced remedial therapist will normally be able to detect these knots through palpation or touch alone, but often will also require verbal feedback from the client in order to confirm whether a sore spot is being pressed upon. Trigger points can be caused by repetitive overuse, over strain, stress, injury, accident or trauma. These knots impede the flow of fresh blood to the area where the knots are, this constriction also means that metabolic waste and toxins which are normally flushed away back into the circulatory system cannot escape so there ends up being a build up in this confined area which is what causes the pain. Trigger points may need to have pressure applied to them in order for the pain pattern to become activated or the trigger point may be in such a state that it is always actively causing the pain regardless. The muscle knots that form a trigger point site do not tend to respond to standard kneading type massage movements, they require precisely aimed static pressure, pressure which shouldn’t be too hard either as this will just make the muscle go into further contracture and hardening. I usually apply up to 12 seconds of constant static pressure on a trigger point, within that time frame the client should be experiencing levels of pain no greater than a 7 out of 10 (and much less is fine), before that time is up I would expect the client to perceive a change in the quality of pain, either getting less or changing say from a sharp pain to dull ache and this would be a sign for me to cease pressing. I could also choose to follow the movement of the tissues as they begin to ease and release, so combining a myofascial release technique (more on myofasical release in an upcoming article).
The most distinctive attribute of most trigger points is their ability to refer pain, so that pain appears to be experienced at a remote and apparently unrelated location to that of where the trigger point actually physically is. Not only are most trigger points able to set-up pain referral conditions, but all these pain referral patterns have been proved by research to be consistently reproducible and predictable. Books and charts have therefore been produced showing typical trigger point locations on a diagram of a muscle along with the expected pain referral pattern(s).
There has been plenty of scientific and medical research conducted into the efficacy of trigger points, but despite this it is still not part of any of the qualifying training that a conventional medical doctor would go through, so therefore most would be ignorant of this phenomenon. Dr Janet Travell who was also president John F Kennedy’s personal physician, was one of the main pioneering figures behind research into the theory and practical implications of trigger points.
Here are so common examples:
Reoccurring headaches where the pain is usually felt in the same predictable areas on the skull every time are usually caused by trigger points in the muscles either side on the side of the neck.
Sciatica and the characteristic shooting pains down the back of leg is often caused by trigger points in the gluteal region muscles and the resulting nerve entrapment that occurs of the sciatic nerve (usually the piriformis muscle deep in the mid region of the buttocks). Can also cause lower back pain issues.
Shin splints are usually usually caused by trigger points in the (tibalis anterior) muscle on the outside front part of the lower leg just a few inches below the knee.
Tingling or numbness sensations in the fingers often accompanied by RSI (repetitive strain injury), carpel tunnel or thoracic outlet syndrome type symptoms are usually caused by nerve fibres (of the brachial nerve plexus) being entrapped by tight muscles containing trigger points, namely the muscles at the base of the neck (scalenes) and the muscles in the chest area either side on the front of the rib cage just a bit below the collar bone (pectoralis minor).
This website I came across whilst researching this article gives an excellent extract from a book about trigger points, but provides an even fuller commentary than here if you are interested in reading more, so I’d point you there for further reading as it’s really very good and saves me from trying to re-invent the wheel here so to speak:
http://saveyourself.ca/tutorials/trigger-points.php
And to see pictorial diagrams and a very comprehensive listing of pain related symptoms that can be related to trigger points in a certain muscle, have a look at this highly informative website:
Here are 2 books that I use myself during client consultation sessions and come highly recommended as well if you are interested in looking into self treatment (click on the images for more details):
Trigger Point Therapy for Myofascial Pain – Fernando & Fernando:
The Trigger Point Therapy Workbook – Davis & Davis:
Thera cane: an essential self treatment tool (comes with instructions)
Soft tissue pain: are you in the 40% group?
A study into the prevalence of significant physical aches, pain and discomfort among the general population showed that…
60% are relatively “pain free” on a day to day basis;
30% experience some kind of accute or regional / local pain;
10% suffer with some degree of widespread distributed pain everyday.
Therefore 40% of the general population experiences some kind of on-going physical pain on-going in their bodies.
Within that 40% group, between 70% – 80% of pain has been found to be soft tissue related in nature. Soft tissue includes the muscles, tendons, ligaments and all pervading connective tissues (known as the “fascia”) of the body.
Massage therapists who have had specalist (usually extended) training in remedial massage and soft tissue manipuation techniques are particuarly well placed to provide effective assistance in the addressing or easing of soft tissue pain. Suitably qualified therapists will usually advertise their skills by using any one of the following modality descriptions in order to differentiate themselves from those who are just offering non-remedial general relaxation massage or spa type treatments: remedial massage, remedial bodywork, sports massage, soft tissue manipulation, soft tissue therapy, myofascial release, fascial bodywork, structural bodywork, structural integration, Rolfing, neuromuscular therapy, neuromuscular technique, neuromusuclar massage, deep tissue massage, trigger point therapy, medical massage and clinical massage. Also related are the modalities of visceral manipulation, craniosacral therapy and physical therapy.
This type of therapy involes various types of postural, visual and functional assessment procedures which help the therapist identify the issue. The work is often concentrated on a particular area with precision focus for an extended amount of time involving interactive feedback with the client, whilst other areas of the body which may seem unrelated to the presenting issue can also be worked on in the same session or in future sessions. Finally the client is given useful exercises to do in-between visits in order to maintain, supplement and enhance the effectiveness of the work done durinig each session.
The video below is aimed at therapists but still will be very much of interest to a lay person such as maybe yourself who may be looking for a proven alternative or complementary approach to relieving their soft tissue related pain, it expalins the physiological mechanism of pain and how remedial massage modalities can help:
Over the next few days, I’ll be publishing a series of articles defining some of the soft tissue modalities and techniques (mentioned above) that I use in my own clinical massage clinic here in Exeter (UK) and how in practical terms they have worked successfully on real world clients.



